SPACE
Hospitals’ strategies regarding how to use space were often innovative and showed proof of adaptability, which made it possible to handle the challenges of the physical environment. Relocation and repurposing were frequently the answer.
Resilient organisations understand how hospitals can adapt and grow through the current pandemic. The study below aims to share information between professionals for a better future resilience.

The Relocate, Repurpose, Reorganize project is fundamentally about learning from the hospital experience of the COVID-19 pandemic, to provide some guidance on how hospitals and health systems can become more resilient. To do this, it focuses on Staff, Systems, Space and Supply chains.
The four project partners are Ramboll, Comentum, White arkitekter and the European Health Property Network. Together, they represent expertise in healthcare architecture and engineering, process and system redesign, health policy and healthcare capital asset investment. They collectively have interests in the design of physical and digital healthcare infrastructure, the links between the built environment and the safety, quality and efficiency of clinical processes. They also have expertise in the costs associated with different environment and care models, change management and how to ensure sustainable improvements in healthcare systems.
Ramboll is a leading engineering, architecture and consultancy company founded in Denmark in 1945.
Ramboll employs 16,500 people globally and has especially strong representation in the Nordics, UK, North America, Continental Europe, Middle East and Asia-Pacific. We are present in 35 countries and combine local experience with a global knowledge base, constantly striving to achieve inspiring and exacting solutions that make a genuine difference to our clients, end users and society at large. Ramboll works across the following markets: Buildings, Transport, Water, Environment & Health, Energy and Management Consulting.
You can find out more about Ramboll here.

Stockholm-based Comentum specializes in change and innovation management in healthcare and the life sciences. We work with hospitals and healthcare organizations in Sweden, Norway and Switzerland. We enable organisations to succeed with strategic projects that matter. We help focus on the right things by sustainably integrating innovation throughout. Our clients share our enthusiasm for sustainable initiatives at the intersection of behavioural, process and technological change.
Together with our clients, we co-create change processes that energize and provide focus to achieve impact. We focus on structuring the organizational development in connection with large-scale building projects in healthcare and life science. This includes the set-up of project offices and innovation frameworks. We help you with user involvement - both employees and patients - and with testing the future way of working before the move.
There are great ideas out there that have the potential to make healthcare a better place for patients and those who care for them. Let us capture them! The expertise and experience of healthcare professionals are the biggest assets for transformations in healthcare. Let us catalyse them!
You can find out more about Comentum on www.comentum.co
If you wish to get in touch directly please reach out to Micha Kämpfer (CEO) via micha.kaempfer@comentum.se.

White Arkitekter is one of Scandinavia’s leading architectural practices. We work with sustainable architecture, urban design, landscape architecture and interior design for current and future generations. Our mission is to enable sustainable life through the art of architecture. Our vision is that by 2030 all our architecture will be climate neutral, through design excellence.
We work with sustainable architecture, design and urban development in an international context. We need to act responsibly, as our work affects the lives of many both present and future generations. We create spaces for people to thrive and grow in harmony with the ecosystem that we inhabit. We act responsibly by operating within the sustainable limits of our planet when we design healthy living environments that inspire and engage.
Our curiosity is reflected in the way we work. We believe that the search for new knowledge will strengthen our offer for the future. Therefore, we continuously invest in research and development. Through design, creativity and a humanistic approach, we look to solve great challenges. We believe that architecture is shaped by the unique qualities of its context. This makes us radical contextualists.
We are an employee-owned company, and we value involvement and participation. We respect the equality of every individual, and we believe everyone has the right to a sustainable life. This is the foundation of our architecture and our culture. Our projects evolve in collaboration with our clients, users, partners, colleagues and other stakeholders.
By being good listeners, understanding varying perspectives and being devoted to collaboration, we create lasting value.
You can find out more about White Arkitekter here.

The European Health Property Network (EuHPN) exists to pool the knowledge from its member organisations to promote a better understanding of how to plan, design, build, maintain and finance all kinds of health facilities, from the largest university teaching hospitals to the smallest clinics and primary care centres. Our members represent interests in healthcare architecture, healthcare capital asset investment, health facility design research and health estate development. The network currently has around 20 member organisations from a range of European countries, plus associate individual and organisation members.
You can find out more about the EuHPN here.
The partner organizations, which provided pro bono resources to make the project a reality, and are grateful for additional financing provided by the following institutions:
Ramboll Foundation, Denmark
Forum Vårdbyggnad, Sweden
White Research Lab, Sweden
Jonathan Erskine - European Health Property Network
Bo Rytkjær Callesen, Flemming Schmidt, Katarina Ringstedt, Michael Stevns - Ramboll
Micha Kaempfer, Anne Richter - Comentum
Jetri Regmi - World Health Organization
Andrea Brambilla - Politecnicodi Milano
Christopher Shaw - Architects for Health
Liesbeth van Heel - Erasmus MC
Charlotte Ruben, Christiana Caira, Saga Karlsson - White Arkitekter
Susan Grant & Michael Cassells - NHS
Ana Maria Alvarez - Pinearq
John Avdoulos & Camilla Moretti - HKS
Pilosof Nirit - Cambridge University
Björn Hollström - Region Stockholm
Birgitte Gade Ernst - Arkitema
Eduardo Teran - Estudio 15arquitectos
Amie Shao - Mass design group
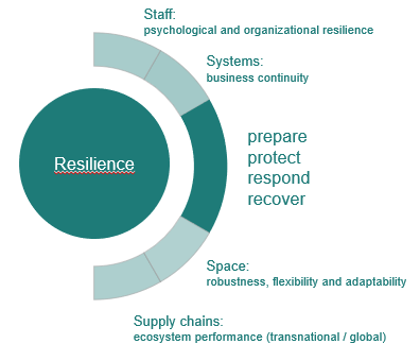
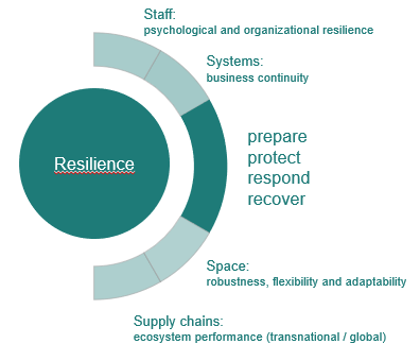
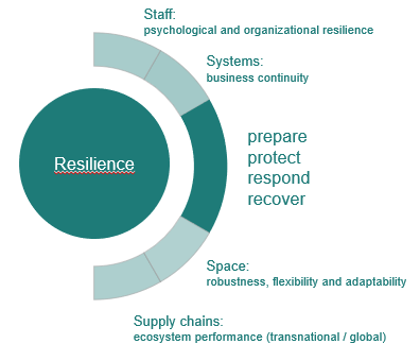
The Relocate, Repurpose, Reorganize project is fundamentally about learning from the hospital experience of the COVID-19 pandemic to provide guidance on how hospitals and health systems can become more resilient. To do this, it focuses on staff, systems, space and supply chains.
From early in the pandemic, resilience became the watchword across global health systems, referring first to the ability of hospitals and public health systems to respond to the first wave of the crisis and later to their capacity to return to normal functioning.
From our desk research, the project team adopted the following working definition of resilience: the capability to maintain and adapt critical functions when faced with changes.
The project uses desk research, regularly updated, to scan emerging literature and intelligence in each of the four focus areas. In addition, it builds a library of case studies to offer insights into the responses of hospitals and health systems in disparate countries and contexts.
Taken together, the desk research references, the case studies and the web-based field guide are a resource for everyone involved in learning how to make hospitals and health systems more resilient to future crises in public health.
As the COVID-19 epidemic unfolded across the world, healthcare systems in general, and acute hospitals in particular, had to make urgent and radical adjustments to the capacity, processes and care models for diagnosing and treating patients. The impact was felt across the system, but especially strongly in departments dealing with emergency, critical and respiratory care.
The response in hospitals encompassed every aspect of the organisation: the physical layout and arrangement of space, how staff should work, the nature of the systems (including IT and communications) that support clinical and non-clinical work and the capability and capacity of supply chains to ensure that equipment, drugs and medical devices were available.
As underlying concepts and assumptions were necessarily uncertain and solutions had to be found at speed, the project partners kick-started learning by taking the opportunity to compare the arrangements found in diverse countries and organisations. A mix of desk and case study research was used to examine all four areas of space, staff, systems and supply chains and to synthesise the lessons learned into a web-based field guide. The overarching aims were to learn from the varied experiences of hospitals and health systems, to make this knowledge available to all and to contribute to building hospital and health system resilience.
The project has four main goals:
The project partners conducted rapid desk research in March and April 2020 to examine the hospital sector’s response to the first wave of the pandemic.
In relation to hospital infrastructure, this revealed common patterns across many countries:
In addition to changes to the built environment, the partners also noted that staffing, systems and supply chains were areas of major disruption and change. Based on these early observations, the partners agreed to conduct further desk research and to seek a broad range of real-world case studies. The desk research used purposive sampling of the rapidly emerging academic and practitioner literature, with contributions from all the partner organisations. The case studies, which mainly focused on Europe and North America, were chosen for the insights they could provide in relation to the ‘4Ss’ – staff, systems, space, supply chains—within the overall context of hospital and health system resilience. The case studies reflect a range of health system types and encompass acute and teaching hospitals of different sizes and organisation types.
Many of the case studies were presented and discussed at four international webinars. The outputs’ combination of case studies and desk research formed the basis of this web-based field guide, with four main goals:
The field guide is an open access resource, intended to help hospital organisations, policy makers, health system planners, architects, engineers and clinicians make choices about how to organise space, staff, systems and supply chains to meet the ongoing challenge of the COVID-19 pandemic and future public health crises. It is a framework for enquiry and discussion, not a set of definitive answers.
Hospitals’ strategies regarding how to use space were often innovative and showed proof of adaptability, which made it possible to handle the challenges of the physical environment. Relocation and repurposing were frequently the answer.
The most sensitive area when it comes to capacity management. With sufficient capacity in staffing and when (re)educating, there is a substantial possibility of recovery and transforming into a well-functioning and adapted organisation and chain of command.
Vital for resilient health care from a global and a micro perspective within a hospital. Many countries are about to change their overall strategy for supply chains to became more resilient in crises.
Not only technical ones but also systems which are part of medical operations or their support. Changes need to rapidly escalate, and digital functions have become invaluable. Learn how facilities systems and MT systems transform and develop together.
Since the first outbreak of COVID-19, registered in Wuhan, China in December 2019, the pandemic has spread globally and continues to do so. The pandemic has had a substantial impact on society. It has required an increased capacity and thus needed to rapidly extend departments.
The changes in requirements for capacity and capabilities have been handled and accommodated with varying speeds and stringency across healthcare systems around the world, but one thing has been globally united: resilience in response to the changing conditions of the pandemic. This has required a rapid ability to track changes and respond to new developments.
There is never a wrong time to learn from each other.
COVID-19 has posed an intense challenge to the healthcare sector – a challenge the world has not seen in decades. This has resulted in the need for a broad range of actions to keep the healthcare systems viable: radical changes to procurement and logistics processes, retraining and reorganizing large numbers of staff and rapid distribution and management of a variety of equipment and technology platforms.
As the seriousness of the situation created by the pandemic grew exponentially on an international scale, it became clear that a multidisciplinary approach to fighting the pandemic would be necessary. Consultants from various sectors and disciplines offered their professional assistance to support their local healthcare systems. At this stage, Ramboll and Comentum, realizing that the situation was overwhelming the local systems, identified the need for gathering and sharing healthcare organizations’ learnings from the crisis; thus the idea for the field guide project was born. We contacted the European Health Property Network (EuHPN) to discuss the project idea and how to engage key stakeholders in the healthcare sector. Just two weeks after in April 2020, the Relocate, Repurpose, Reorganize project (3Rs, for short) was initiated. In the first webinar, the overall ideas of the project were tested:
At this point, we applied for and were granted DKK 375,000 in funding from the Ramboll Foundation that supports non-commercial ideas to benefit society.
The first webinar was held on 29th May 2020 and was a great success with over 150 international attendees. Five cases from Switzerland, Sweden, Scotland, the United States of America and Spain were presented and discussed.
In the following weeks, White Arkitekter joined the project team, providing additional funding for the project (White Research Lab, 215 000SEK).
We have organized five webinars during the last ten months – each focusing on a different aspect of hospital resilience – to increase our understanding of how hospitals can be made more resilient and to provide this knowledge to healthcare providers all over the world in their attempts to prepare for the future.
More specifically, this project has had the following goals:
Throughout the process, we have had the privilege of collecting a wide variety of cumulative knowledge:
We have profited greatly from the different competencies brought in by the different project partners. What we have learnt throughout the research and publication phase can be summed up as follows: most publications focus solely on the physical (space) alterations or take a purely medical perspective on the challenges COVID-19 placed on healthcare systems worldwide. Another stream of publications gravitates around the topic of psychological impact on staff and patients. We believe that through our multidisciplinary approach we are able to build bridges between the different facets of resilience, from the individual to the healthcare ecosystem as a whole.
Our overall findings from the project presented in the chapters of the field guide:
Resilience related to staff:
The pandemic has forced rapid changes to clinical processes and the built environment, which has had major impacts on behaviours, relationships and expectations for individuals, teams, departments and the whole organization, particularly in relation to issues of dislocation, isolation, working practices and management relations. Staff well-being has been a critical area of focus, and it is clear that most hospitals must sustain and increase their resources to support staff well-being.
Resilience related to healthcare and hospital systems:
To effectively respond to crises through the reorganization of systems to manage new conditions while maintaining core functions has been a great challenge. The pandemic has challenged systems on different levels (national and organizational). To ensure the proper functioning of integrated care, special COVID-19 command centres and redefining roles and responsibilities through the integration and extension of capabilities have been used. Technical systems, necessary to maintain medical operations and the vital functions of hospital buildings, are also included in our study. Adaptability is the key; however, to a great extent, the technical systems have been able to withstand the pressure during the crisis.
Resilience related to physical space:
Hospitals have been applying different strategies to transform and adapt the built environment, depending on the local organizational, technical and geographical conditions. Four categories of transformation and adaptation were identified: non-healthcare buildings, existing hospitals, newly completed hospitals, plug-in spaces to existing hospitals.
Resilience related to supply chains:
Numerous supply chains have underperformed or were over-stressed during the pandemic. Solutions are characterized as local, national or global, and they focus on the coordination and security of personal protective equipment for primary and secondary healthcare organizations, the establishment of national coordinated action for medical supplies and the coordination between nations.
Overall conclusion and implications:
Hospitals have responded to the pandemic effectively and creatively, despite major challenges. Nonetheless, in many cases, the crisis has forced a re-evaluation of the working practices, the support for staff well-being, the infection control design of hospital, the effectiveness of existing systems and the operational resilience of supply chains. These issues must be urgently addressed at local, national and international levels.
Jeffrey Braithwaite, BA, MIR (Hons), MBA, PGDipLR & the Law, PhD, FIML, FCHSM, FFPHRCP, FAcSS, Hon FRACMA, FAHMS
From the earliest times healing has been an important human practice. Every recorded culture had some kind of care, medicine, and treatment for those suffering from illness, injury or misadventure.
Eventually, a place emerged where people could go to access a concentrated set of expertise to care for them. The earliest healing institutions are first documented by a Chinese Buddhist monk in around 400 AD in what is now India. Such healing institutions over the millennia became what we now have been able to recognise increasingly over the last 200 years, and especially in the 21st century, as hospitals. True enough, there was also caring in the community across the centuries, but it was mainly centred on individuals as historically, a public health response was lacking – we simply did not know how to deal with large-scale crises such as pandemics until relatively recently.
In the last couple of centuries the more recent history of hospitals tells a story about increasing technology and advancing and more sophisticated clinical and caring practices. Now we have modern citadels, the largest of which are essentially small cities in their own right, offering a world of care, diagnosis, treatment and procedures so as to deal with a bewildering range of illnesses, infections and diseases. The modern hospital is also linked to public, environmental, general practice, aged care, rehabilitation and other kinds of services which are outside its walls. Because of innovations in information technology, the age of networked connectivity amongst providers is upon us.
Millions of people have benefited from these technological and procedural advances such that diseases which were once considered terminal – heart conditions, cancer, a vast array of illnesses and disability associated with aging – can now be ameliorated. Whilst this is very much the case, in a very noticeable 1:10 of episodes of care, and sometimes more, patients suffer an adverse event and a proportion of those, major harm. So while clinical progress has been considerable and often inspiring, there is still much to do to create high quality, safe care for all.
What we know is that technology will continue its inevitable march and science will contribute increasingly to better, more technologically-enabled caring systems. Practices and procedures will improve, too. This is not just because historically there has long been an improvement gradient as far back as we can see, but that a sophisticated society which cares for its citizens will always have ambitions to do better over time.
The ultimate aim of these continuous efforts to improve is to have a hospital of the future which is smart, connected and person-centred, and which can deal effectively with whatever care is needed to be provided, no matter how rare or commonplace, challenging or routine, or costly or inexpensive. It is a hospital system which makes care available universally, to all who come to it in need. The main building blocks to underpin this motivating vision for the future hospital are two-fold: technological (buildings, effective information technology, clinical and diagnostic capabilities) and behavioural (state of the art practices, procedures and techniques). The former is all about science and the application of technology; and the latter is all about professional practice, teamwork and resilience in the face of challenges which all health professionals face.
Armed with this blueprint for the future, this field guide, Hospital resilience in the face of a pandemic: Learnings from the first wave of COVID-19, canvases a wide range of cases, ideas, conceptual frameworks, expertise and fieldwork to consider best practice across the entire spectrum, including resilient performance, staffing and staff innovations, the well-being of providers, supply chain and logistics, systems of care, repurposing and the idea of new spaces for hospitals of the future. It is written by some of the leading figures in design, management, planning, governance, architecture, engineering and policy.
The work represents a unique assemblage; a bringing together of core ideas from which we can all learn about the hospital of the present and resilient performance and the way these can help shape our thinking so we can provide improved care across the rest of the 21st century and beyond. It is destined to become a guide for pandemics of the future, and a star to steer by when new, unexpected crises befall us.
It is hard to think of a more important enterprise than this. I commend the topic, the authors and the content to all who are interested in providing better care to their patient populations, now and in the future.
"Bringing together ideas from which we can all learn from and shape our thinking."