Pandemic Resilience
SPACE ADAPTATION
Healthcare providers have faced a major challenge concerning the built environment of the acute care hospitals - with an insufficient number of patient and ICU beds and new demands to decrease the infection risk for staff, visitors and other non-Covid-19 patients. Hospitals have been applying different strategies to transform and adapt to the built environment, depending on local organisational, technical and geographical conditions.
Introduction
Healthcare providers have faced a major challenge concerning the built environment of the acute care hospitals - with an insufficient number of patient and ICU beds and new demands to decrease the infection risk for staff, visitors and other non-Covid-19 patients. Hospitals have been applying different strategies to transform and adapt to the built environment, depending on local organisational, technical and geographical conditions.
In Autumn of 2020, a new wave of the pandemic is spreading across Europe and the world. Therefore, at the time of writing, it is difficult to draw definitive and complete conclusions. This chapter is based on case studies observed during the pandemic outbreak between Spring and early Autumn 2020. The case studies have been presented and examined during the Reorganise, Relocate, Repurpose series of webinars.
In this chapter, you will learn the following:
- how buildings have been transformed to meet the new demands
- lessons learned regarding the pandemic resiliency of the built environment
The following strategies are described as common components of the response in several countries and are supported by different case studies:
Transformation strategies
1. Transformation of non-healthcare buildings
Find more →
2. Transformation of hospitals
Find more →
2A. Transformation of newly completed hospitals
Find more →
2B. Transformation of existing hospitals
Find more →
3. Plug-in spaces to existing hospitals
Find more →
4. Implementation of ongoing projects and new initiatives
Find more →
Background
Physical, economical, technical, organisational, social and legal changes are inevitable[1] in a hospital building which is often expected to withstand between 50 and 100 years.[2] Designing a hospital is one of the most challenging tasks for a project group working with the built environment. Larger hospital projects have lengthy design processes[3] (up to 20 years) and can include up to a thousand project members. During the design process, project members are often asked to solve a program with hundreds of rooms and advanced technology; at the same time, the future hospital should have a healing environment where both patients and the staff’s well-being are prioritised. Additionally, the planning and designing of the hospitals are both impacted by changes of the healthcare organisation using it but are also often designed to be adaptable for future changes.
Nevertheless, the Covid-19 pandemic has been one of the most challenging periods in the modern history of hospital planning. The situation has forced organisations to act fast. This has entailed creating entirely new modular hospitals, adding extensional spaces to hospitals, transforming existing hospitals or even transforming non-healthcare buildings, such as exhibitions halls, sport halls and convention centers into healthcare facilities, in some cases in only a matter of days.
The growing trend for the design processes of hospitals is to rely on evidence-based design (EBD). EBD can be described as ‘design that is informed by a deep knowledge of research and commitment to add to knowledge base through careful evaluation and information sharing.’[4] EBD has also been described as a process wherein the decisions are made in combination with (1) credible research evidence, (2) organisation/population needs/preferences/resources and (3) practitioners’ design expertise; this is all situated in an ecological context (organisation, culture, social and physical environment).[5] The use of EBD during the design processes of healthcare buildings can benefit key stakeholders such as patients, families, physicians, nurses, other staff and healthcare organisations,[6] since the healthcare building plays an important role in both the healing process of patients and the working environment of staff.
The needs of the key stakeholders are one component in the design process; however, another important factor is the impact of healthcare buildings on the global environment. According to the WHO, health services account for 5 to 15% of carbon emissions in developed countries,[7] and healthcare buildings are a major contributor to this figure. Therefore, in today’s healthcare building design process, sustainability goals are high priority; there is a focus on both reducing the impact on the global environment and increasing the length of use.
With the help of strategic design solutions, project members aim to prepare healthcare buildings for future changes;[8] the resulting differences in design solutions create different initial positions and possibilities to meet challenges such as a pandemic.
Cases
During the Reorganise, Relocate, Repurpose series of webinars, we found a diversity of solutions when adapting the built environment to the new pandemic. One conclusion is that the given solution is a combination of organisational possibilities as well as the availability and standard of existing healthcare facilities in each country or region.
The transformation of non-healthcare buildings was used in many cases as a first emergency strategy at the beginning of the pandemic. This strategy is a solution for healthcare providers to place the pandemic care outside of hospital sites but still use an existing structure. In this study, we have identified six cases: Louisa Jordan Hospital (Scotland), USACE Novi (USA, Michigan), Stockholm fair (Sweden), Sport facility Hospital del Mar (Spain), Ifema exhibition center (Spain) and Sheba Medical Center (Israel). The strategy has typically been applied to exhibition halls, sport halls, conventions centers (Louisa Jordan, USACE Novi, Stockholm Fair, Ifema), as well as a parking garage within a medical center (SMC Israel). With the help of prefabricated modular systems, which are easy to assemble and disassemble, a substantial increase in the number of ICU beds could be achieved in a brief amount of time.
The six cases presented in this study include an escalation strategy and have been based on the early projections of the number of ICU beds needed.
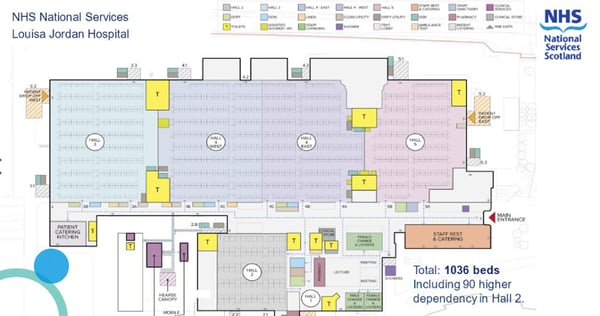
Picture. Louisa Jordan Hospital, Glasgow, Scotland was planning to have 1,036 beds, but in the first phase only 300 beds were built.

Picture. Louisa Jordan Hospital, Glasgow, Scotland
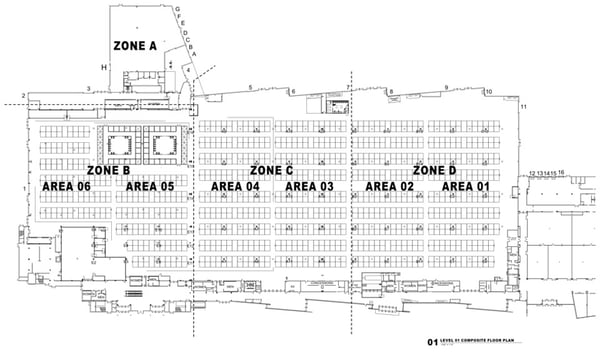
Picture. USACE Novi, Michigan, USA was planned and divided into four zones. After 6 days, the first phase of 250 beds was completed

Picture. USACE Novi, Michigan USA
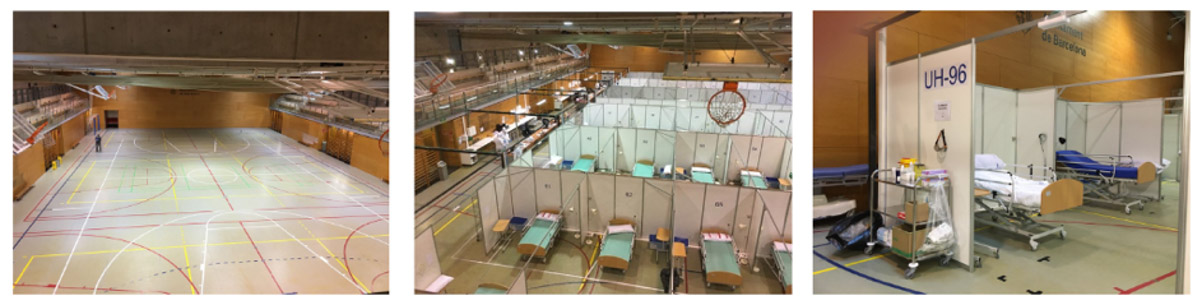
Picture. Hospital del Mar, Barcelona, Spain. Emergency extension in a sport facility close to the hospital. The transformation of the sport facility lasted less than a month. The existing beds and the minor transformations made inside the main hospital was enough to assist the patients in the peak of the pandemic.
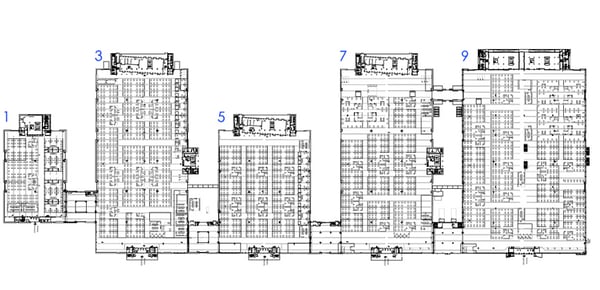
Picture. IFEMA Exhibition Centre, Madrid, Spain. Pavilions were available to locate the different hospitalisation areas.
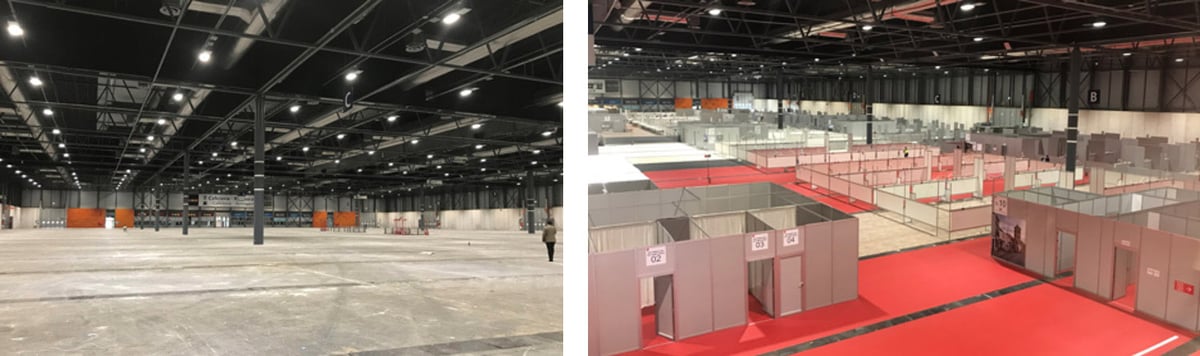
Picture. IFEMA Exhibition Centre, Madrid, Spain. Before and after picture
Advantages of non-healthcare buildings
- Large buildings with several entrances and few internal walls enable high flexibility for arranging suitable flows.
- The existing infrastructure around the existing buildings eases access for both ambulances and deliveries of new systems and supplies.
- Possibility to control access to the buildings to ensure that only authorised staff can enter and exit.
- One of the fastest solutions for a substantial increase in patient beds.
- The temporary room layout often includes several patients to be treated in the same area, which eases staff overview of patients.
Disadvantages of non-healthcare buildings
- Covid-19 care separated from hospitals is a disadvantage for patients who needs access to other healthcare services.
- Challenging to staff these structures, due to physical distance to hospital buildings.
- Risks and challenges to install medical gas and energy supplies which were not designed for it.
- The temporary environment often lacks basic elements of healing environment, such as daylight, privacy, good acoustics etc. for both staff and patient.
- Psychological impact on patient when being treated close to others – study shows that blood pressure may increase in patients who observed what was happening to others.[9]
Cases
2
Transformation of
Existing hospitals
Another strategy that has been widely applied, sometimes in combination with plug-in spaces (see strategy 3), has involved transforming existing hospitals. Generally, the goal of this strategy has been to place Covid-19 care within the hospital structure to access staff and to benefit from existing logistics and infrastructure. This strategy has often been connected to the decision to partly pause or postpone normal healthcare provisions, such as elective surgeries or outpatient care. This is also a strategy that has resulted in a substantial increase in ICU beds, but within the existing hospital building.
The possibilities of transformation have been highly dependent on the flexibility and the technical standard of the buildings. Therefore, this chapter has been divided into two: (2A) transformation of newly completed buildings and (2B) transformation of existing older buildings.
During the last 20 years, many hospitals in Europe, specifically in northern Europe, have been undergoing major changes with extensive refurbishments or extensions. The Erasmus MC (Netherlands), New Karolinska Solna (Sweden) and several new general hospitals in Denmark (Aarhus, Odense etc) are some examples. The access to newly completed buildings made it possible for some hospitals to quickly redirect these facilities to Covid-19 care.
In this study, we have identified two cases: New Karolinska Huddinge (Sweden) and Rigshospitalet in Copenhagen (Denmark). Both are buildings designed for surgery departments that were converted into ICU wards for Covid-19 patients. Spaces such as operating theatres and post- and pre-surgery rooms were selected because they were from the beginning prepared to meet the advanced technical standards and therefore easy to transform into ICUs. The rooms are also larger in space, in comparison to standard patient rooms, so that every room can accommodate several beds. This solution would enable the medical team to overview several patients at the same time.
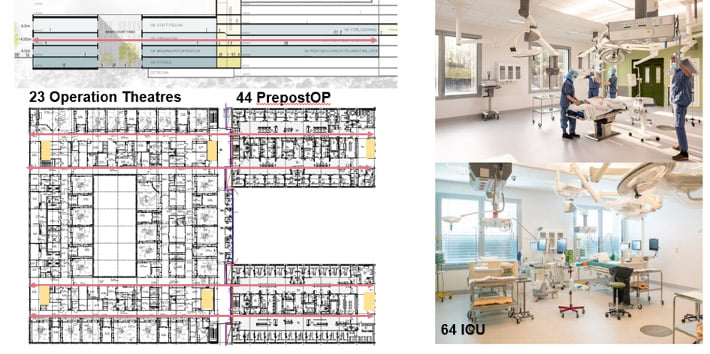
Picture. 23 surgical theaters and 44 pre/post surgical beds were transformed into approx. 64 ICU-beds for Covid19-patients.
Picture. O-huset, New Karolinska Huddinge, Stockholm, Sweden.

Picture. Rigshospitalet, Denmark. Preparation of new rooms for Covid-19 patients. Photo: Rigshospitalet.
Advantages of newly completed hospitals
- Good working environment for staff: daylight, views and well-planned staff rooms compared to many solutions observed in strategy 1.
- Staff have access to the latest advanced technology.
- Access to all logistics and infrastructure within the hospitals.
- Easier to staff due to adjacent hospital.
Disadvantages of newly completed hospitals
- Challenges in separating entrances, horizontal and vertical flows within the building.
- Partial postponing of normal healthcare provision, such as elective surgeries or outpatient care. This created a ‘care dept’ (currently a discussion in many Swedish Regions).
Cases
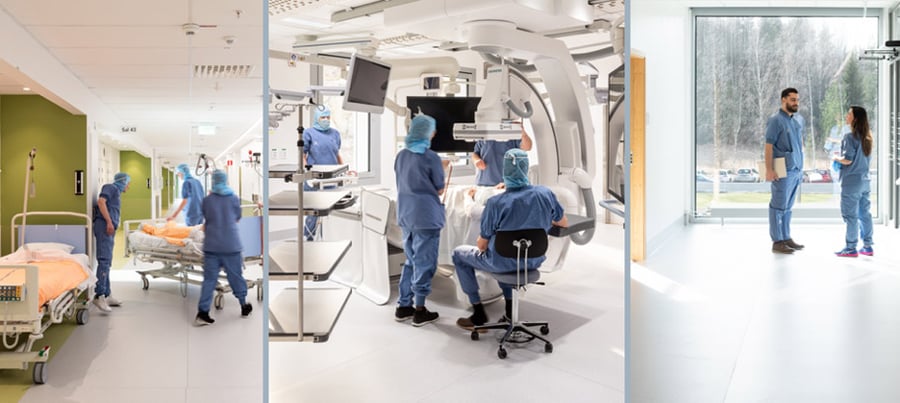
Hospitals are typically designed to be flexible. Existing hospitals, from older structures to more modern, were adapted during the Covid-19 pandemic to increase the number of ICU beds and separate the flows within the buildings, in order to decrease the risk of the pandemic spreading within the hospitals. In general, these solutions were intensively used and often successful in terms of treating Covid-19 patients. In this study, we have observed three cases: Mount Sinai Hospital (New York, USA), Mother-Child Clinic at Slagelse Hospital (Slagelse, Denmark) and Hospital del Mar (Barcelona, Spain).
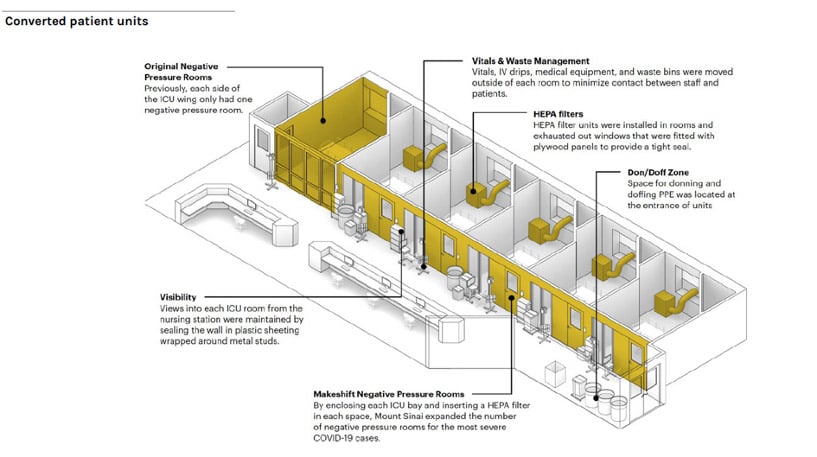
Picture. Mount Sinai Hospital, NYC USA. Converted patient rooms for Covid-19 care.
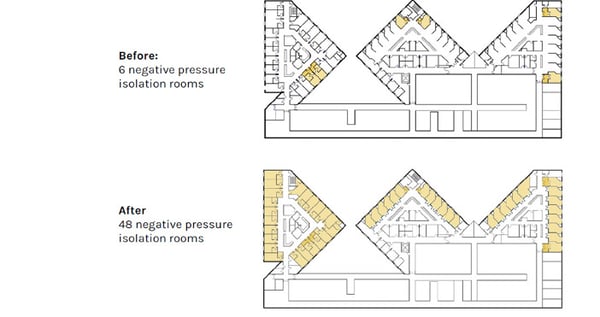
Picture. Mount Sinai Hospital, NYC USA. The number of negative pressure isolation rooms before and after adaptation.
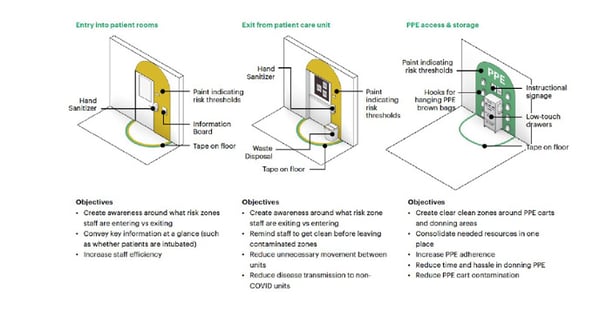
Picture. Mount Sinai Hospital, NYC USA. Design hacks to help staff understand their environment
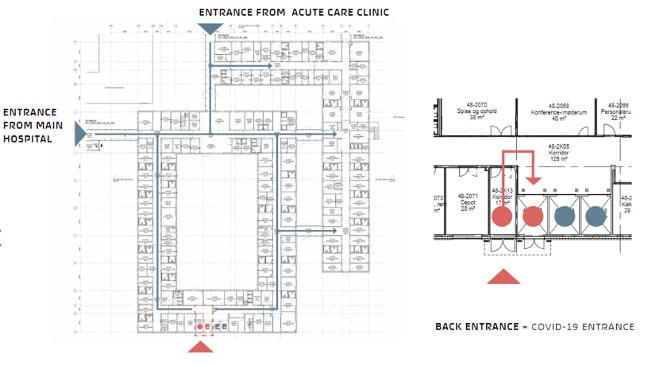
Picture. Mother-Child Clinic at Slagelse Hospital, Denmark. Separation of Covid-19 entrance and flows.
Advantages of existing hospitals
- Depending on the building standard: better working environment for staff compared to many solutions employed in strategy 1.
- Depending on the building standard: staff have access to the latest advanced technology.
- Access to all logistics and infrastructure within the hospital.
- Easier to staff due to adjacent hospital.
Disadvantages of existing hospitals
- Depending on the flexibility of the building, more or less optimal solutions for Covid-19 care
- New spatial grammar and zoning of the wards can be difficult to understand for staff.
- Challenges in separating entrances, horizontal and vertical flows within some buildings.
- Partial postponing of the normal healthcare provision, such as elective surgeries or outpatient care. This created a ‘Care Dept’ (currently a discussion in many Swedish regions).
Cases
Plug-in spaces to existing hospitals are another strategy that has also been widely applied, mostly in combination with the transformation of existing hospital buildings. The possibilities to add plug-in spaces have been highly dependent on the availability of this type of solution but also on the access to free space in a convenient place within the hospital site. In this study, we have found five different plug-in spaces case studies: the extensions of Sahlgrenska University Hospital (Gothenburg, Sweden), Rigshospitalet in Copenhagen (Denmark), Hospital del Mar (Barcelona, Spain), Mount Sinai Hospital (New York City, USA), Slagelse hospital (Denmark).

Picture. Rigshospitalet, Copenhagen, Denmark. Covid-19 test center. Photo: Lars Wallin

Picture. Mount Sinai Hospital, NYC USA. Additional tents in Central Park.
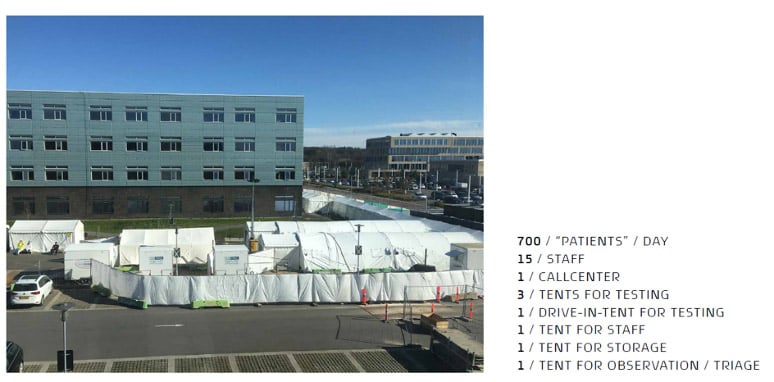
Picture. Slagelse hospital, Denmark. Tents outside the mother and child clinic.
Advantages of plug-in solutions
- Provisory modules (triage tents) standing outside emergency entrances have been a successful strategy to keep the untested Covid-19 patients separated from other patients before entering the hospital.
- Plug-in spaces such as the Sahlgrenska military tent was a fast means to increase the amount of ICU-beds.
Disadvantages of plug-in solutions
- Temporary spaces such as these lack both good working and healing environment; low standards and limited security for staff, patients and supplies.
Cases
4
Implementation of ongoing projects and new initiatives
In Autumn of 2020, a new wave of the pandemic is spreading across Europe and the world. Therefore, at the time of writing, it is difficult to draw definitive and complete conclusions.
Even if it is too early to conclude lessons learned concerning the built environment, many hospital planners have pursued the challenge of adapting existing hospitals during the pandemic. This has led to strategies in implementing different changes during ongoing projects such as the changes during the design process of SNR hospital Mordmoere og Romsdal (Norway); it has also led to new initiatives such as the Pandemic Hospital in Madrid, Spain.
In the design process of Hospital Nordmoere og Romsdal, the following changes has been incorporated, among others, due to the pandemic:
- Separated pandemic triage entrance at the emergency department.
- Sinks in all observation rooms.
- Vertical separation – acute/pandemic/other
- Separated labs – pandemic/non pandemic
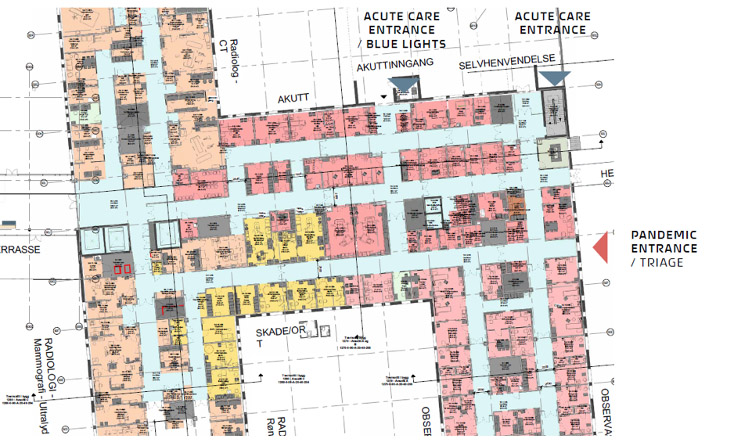
Picture. Hospital Nordmoere og Romsdal, Norway. Separated pandemic entrance at the emergency,
In Madrid, the General Director of Infrastructure of the Regional Department of Health of the Community, has taken one step further than most regions. Madrid is currently building a new pandemic hospital with the aim of taking care of future emergency situations and of coordinating and engaging medical alarms or catastrophes. The complex will also function as a hospitality and logistic centre for medical resources.

Picture. New Pandemic Hospital in Madrid. View from the site.
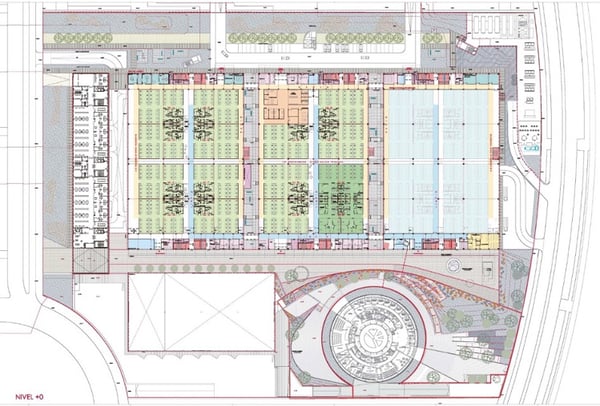
Picture. New Pandemic Hospital in Madrid. Floor plan.
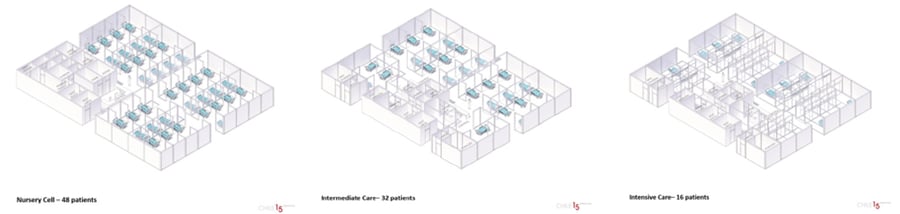
Picture. New Pandemic Hospital in Madrid. Organisation of different cells and units.
Cases
Lessons Learned
During the study, we have observed that various strategies have been applied to adapt the built environment to the pandemic. One observation is that the various strategies depend on different national and regional organisational pre-conditions and decisions as well as the availability and standard of existing healthcare facilities in each country.
The pandemic has found most organisations unprepared. The unpreparedness has been on multiple levels, but regarding the built environment, the major challenges have been to arrange, in a short period of time, a large number of ICU beds and separate Covid-19 flows from other flows within the buildings to protect staff, risk groups and other patients.
In Autumn of 2020, a new wave of the pandemic is spreading across Europe and globally.
Therefore, at the time of writing, it is difficult to draw definitive and complete conclusions. The following lessons learned are based on case studies observed during the pandemic outbreak from Spring to early Autumn of 2020.
Some regions (Västra Götaland, Sweden) are currently developing plans to prepare their hospitals for future pandemics. Some countries are building completely new pandemic hospitals (Pandemic Hospital of Madrid). The challenge of planning for future pandemics is that it is difficult to plan for unknown viruses or infections. For example, the requirements on the built environment might be completely different depending on whether it is an airborne infection.
However, after our study it is possible to draw some conclusions of a general character which are relevant for the resilience of the built environment to future pandemics.
Temporary solutions and extensions
Temporary solutions such as plug-in solutions have shown to be a fast, efficient and flexible means to respond on critical change. These solutions have often been successfully used due to closeness to existing hospital structures (closeness to staff, supplies, infrastructure, etc). The opportunity to use temporary solutions in future pandemics nevertheless requires preparedness on site: hospitals’ master or strategic plans could identify specific unbuilt sites, close to crucial infrastructure such as infection clinics and A&E departments, and reserve them for these kinds of temporary extensions.Non-healthcare spaces reserved for healthcare
It might as well be feasible to develop a strategic plan, national or regional, to identify and prepare dedicated non-healthcare buildings as reserved healthcare spaces for future pandemics. Many case studies show that these structures, although not prepared from the beginning, can be re-organised easily and in a short time due to their flexible structure. This strategy assumes that the healthcare organisations have the preparedness for staffing and supplying the units, which are physically separated from hospital sites.Standards in the healing environment
The challenge regarding both solutions above has been the low standards of the working and healing environment; this has been particularly apparent in the spaces that have been occupied. Specifically the lack of daylight and views to the outdoors have been noticed by both staff and patients as well as a lack of integrity for patients. This reflection might be taken in consideration by future pandemics; if solutions such as those above must be used for longer period, it is crucial to apply principles of evidence-based design for temporary structures.Flexibility and adaptability
In general, temporary solutions as described above can be a part of the answer to future pandemics, independently of the type of infection. It is, for example, improbable that all countries might invest in a larger number of permanent ICU beds in the future due to high costs and lack of staff. The high level of flexibility makes these solutions adaptable to different needs.Flexibility
A general key to success in the adaptation and transformation of existing hospitals is the high flexibility of spaces, layouts and technical supplies. In the specific context of the Covid-19 pandemic, larger rooms with a high standard of technical installations, such as OP theatres, Pre- and post- OP rooms, have been transformed into ICU rooms for Covid-19 patients. Flexibility for future transformation is a demonstrated best practice principle for future-proof and pandemic-resilient hospitals, although it might implicate a higher capital investment in the short term.
Sectionable units
Units and departments might be planned to be divisible in sections, each with separated entrances, if necessary. The possibility to dedicate part of one department to infected patients is a design solution that could be prepared in future projects or existing buildings, when possible. It implicates for example solutions for physical separation through sluices, separation of flows and entrances, separation of technical supplies as well as redundancy in certain functions or rooms.
Separation of flows
It is crucial to design for separated flows of patients, staff and goods, as well as in-patients and outpatients or visitors. This separation applies to both horizontal and vertical flows. It has been a general best practice design principle for post-antibiotic hospitals and has become even more decisive during the Covid-19 pandemic.
Access to multiple entrances
The possibility of separating flows implies that the building and the different units are accessible from multiple entrances. The access to multiple entrances is not obvious because it requires access to multiple elevators and staircases, as well as proper accessibility from outdoor spaces. It is a solution that might in the future contrast with another relevant trend in hospital design: the concentration of few public entrances due to security risks.
Multiple rooms with direct access from the outside
A&E and infections clinics might be planned and re-adapted to have multiple rooms that can be accessed directly from outside. In A&E departments, it has been crucial to separate triage and testing of Covid-19 patients as much as possible from other patient flows. This solution might considerably determine the layout of these units in future hospital projects.
Re-think waiting areas
In general, waiting areas shall be designed to avoid overcrowding. Different solutions might be implemented such as divisible waiting rooms, several smaller waiting rooms instead of central large ones, as well as designing protected outdoor spaces for waiting purposes.
Design for visitors and families
Facilities shall be designed to enable safe visits of relatives and loved ones. This has been one of the greatest challenges during the Covid-19 pandemic, due to the lack of protective gear and proper physical solutions.
EBD
Healing design has been shown to be highly important, or maybe even more important, during a crisis such as a pandemic. Staff and patients have been affected by a highly stressful and unknown situation. The adaptation of newly built hospitals, with high-quality daylight and views, access to outdoor spaces and well-planned staff areas, have exemplified how flexibility goes hand in hand with healing architecture.
References
[1] Schmidt, A. and Austin, S., Adaptable Architecture: Theory and practice, New York, Routledge, 2016.
[2] Karlsson, S., Framtidssäkring i vårdbyggnadsprojekt, Lic., Gothenburg, Chalmers University of Technology, 2010
[3] Olsson, N.O., and Hansen, G.K., ‘Identification of critical factors affecting flexibility in hospital constructionprojects’, HERD: Health Environment Research & Design Journal, vol. 3, no. 2, 2010, 30-47
[4] Ulrich, R., ‘Building the Evidence Base for Evidence-Based Design’, Environment and behavior, vol. 40, no.2, 2008, 147-150; Hamilton, D.K., ‘The four levels of evidence-based practice’, Healthcare Design, vol.3, 2003, 18-26
[5] Peavey, E. and Vander Wyst, Kiley., ‘Evidence based design and research informed design: whats the difference? Conceptual definitions and comparative analysis’, HERD: Health Environment Research & Design Journal, vol. 10, 1937586717697683. 10.1177/1937586717697683.
[6] Ulrich, R., et al., ‘A conceptual framework of the domain of evidence-based design’, HERD: Health Environment Research & Design Journal, vol. 4, no. 1, 2010, 95-114.
[7] World Health Organization, ‘Health and climate action’, 2019, https://www.euro.who.int/__data/assets/pdf_file/0009/397791/SDG-13-policy-brief.pdf?ua=1 , (accessed 8 december 2020)
[8] Karlsson, S., Framtidssäkring i vårdbyggnadsprojekt, Lic., Gothenburg, Chalmers University of Technology, 2010
[9] Inpatient telemedicine for COVID-19: New Model of Care at Sheba Medical Center in Israel, Presenter N. Pilosof, Cambridge, UK, Cambridge Univeristy, 2020, (accessed January 2021)
Credits
Christiana Caira & Saga Karlsson - White arkitekter